Effect of Bracket Slot and Archwire Dimensions on Anterior Tooth Movement During Space Closure in Sliding Mechanics: A 3-Dimensional Finite Element Study
Jun-ya Tominaga et al.
Introduction
The biomechanics of anterior tooth movement, especially in the context of space closure with sliding mechanics, depend heavily on the interaction between bracket slot dimensions, archwire size, and power arm length. This study examines how variations in bracket slot and archwire dimensions impact the type of anterior tooth movement during en-masse retraction. By using a three-dimensional finite element model (FEM), the authors provide insights into optimizing archwire-bracket combinations to achieve desired tooth movements.
Key Concepts
Bracket Slot and Archwire Dimensions:
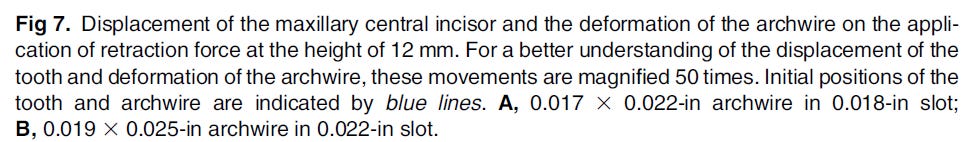
The study investigates two different bracket slot and archwire combinations:
0.018 × 0.025-inch slot with a 0.017 × 0.022-inch archwire
0.022 × 0.028-inch slot with a 0.019 × 0.025-inch archwire
These combinations were assessed to understand their impact on anterior tooth movement, including bodily movement, lingual crown tipping, and lingual root tipping, during space closure using sliding mechanics.
Finite Element Model (FEM):
The authors employed a 3D FEM that included the periodontal ligament (PDL), alveolar bone, maxillary central incisors, and associated brackets and archwires.
The model allowed for precise simulation of the forces applied and subsequent tooth displacement, providing an in-depth analysis of how specific mechanics influenced tooth movement.
Power Arm Length and Retraction Force:
Power arms attached to the archwire were varied in length to assess their influence on tooth movement:
For the 0.017 × 0.022-inch archwire in the 0.018-inch slot, bodily movement of the incisor was achieved with a 9.1-mm power arm.
For the 0.019 × 0.025-inch archwire in the 0.022-inch slot, bodily movement required an 11.6-mm power arm.
The position and length of the power arm were crucial for determining the type of movement (tipping vs. bodily movement), as well as for achieving controlled tooth movement.
Key Findings
Archwire-Bracket Play:
Increased play between the archwire and bracket slot impacted the type of tooth movement significantly:
Greater play was associated with more challenging control over tooth tipping and root alignment, reducing the efficacy of torque application.
In the 0.022-inch slot system, achieving controlled lingual root tipping was particularly difficult due to the larger play, suggesting that precision in slot-archwire fit is crucial for controlled movement.
Influence of Power Arm Length:
Bodily movement of anterior teeth is best achieved by using power arms that extend beyond the center of resistance.
For the 0.018-inch slot system, controlled lingual root tipping and bodily movement could be achieved at shorter power arm lengths. Conversely, the 0.022-inch slot required longer power arms for similar movements, complicating clinical application.
Biomechanical Implications:
Traditional biomechanical principles, which are typically based on static models, may not accurately predict tooth movement in sliding mechanics due to additional forces acting on the archwire-bracket system.
Forces were found to differ from theoretical predictions, suggesting that practitioners should consider the impact of play and archwire deformation when designing treatment plans involving en-masse retraction and sliding mechanics.
Clinical Applications and Recommendations:
Clinicians are advised to use smaller slot sizes and minimize bracket-archwire play when precision in anterior tooth movement is required, particularly in cases requiring controlled root movement.
The study supports the use of high-torque brackets or archwire modifications to compensate for the limitations in torque control in wider bracket slots.
In patients with shallow gingivobuccal folds, long power arms may not be feasible, highlighting the importance of individual anatomical considerations.
Conclusion
This finite element study provides valuable insights into the mechanics of anterior tooth movement during space closure using sliding mechanics. The findings emphasize the importance of selecting optimal archwire-bracket combinations and adjusting power arm lengths to achieve controlled, efficient tooth movement. Orthodontists are encouraged to consider bracket slot and archwire dimensions as critical factors in treatment planning, especially for cases where bodily movement or controlled root alignment is necessary. This study’s detailed analysis aids in understanding how to maximize control in orthodontic space closure, reinforcing the value of precision in biomechanical planning.